We use cookies to improve your experience. By accepting you agree to our cookie policy

You will most likely be aware of the rapidly evolving global health emergency situation in relation to Coronavirus (COVID-19). We are closely monitoring events and are taking advice and information from various relevant sources including the World Health Organisation (WHO), Center for Disease Control and Prevention (CDC), Public Health England and Health Service Executive (HSE) as well as the British Pain Society.
We have written this article on the coronavirus COVID-19 that will be updated as and when new information and guidance is given. However please keep up to date with the U.K. Government and Public Health England’s advice or your own country’s advice.
As of January 2021 the UK Prime Minister placed the U.K. in lockdown until mid-February 2021.
People in England must stay at home and only go out for certain reasons. They have made it illegal to leave your home without a “reasonable excuse”. If you don’t have a reasonable excuse for leaving your home, the police can fine you £200 for a first offence, which will double for further offences up to a maximum of £6,400.
Hopefully our article on Coronavirus (COVID-19) and CRPS will help you understand more about the virus, it’s symptoms and any effects on those living with Complex Regional Pain Syndrome (CRPS) or other chronic illnesses.
If you have CRPS or another chronic condition, and you are experiencing the symptoms of coronavirus COVID-19 and you think you may be infected with the virus, it is crucial you seek medical attention immediately by using the 111 NHS online.
If you are in the UK as of January 2021, if you or anyone in your home has any of the symptoms you and all members of the household are now advised to self isolate. You are advised not to visit the GP, hospital or pharmacy. If your symptoms worsen then you are advised to call 111 or visit the coronavirus NHS111 website to get up to date advice.
For those in the United Kingdom please see further down for the guidance on social distancing for those with underlying health conditions who are at risk of the serious form of the virus as of 10 May 2020.
A coronavirus is a type of virus that can cause illnesses such as the common cold, severe acute respiratory syndrome (SARS) and Middle East respiratory syndrome (MERS).
The 2019 Coronavirus (COVID-19) is a new strain of coronavirus first identified in Wuhan City, China. As a group, coronaviruses are common across the world. However the 2019 Coronavirus (COVID-19) is caused by a member of the coronavirus family but it has never been encountered before.
The World Health Organisation (WHO) has officially named the virus responsible as COVID-19. It was previously known as 2019 Novel Coronavirus. COVID-19 stands for coronavirus disease 2019. The virus also has another name which is severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2).
According to a Chinese research study (Xiaolu Tang et al 2020) of 103 samples of the COVID-19 virus it has been suggested that two (2) main strains have emerged, which have been designated as S and L.
They have also stated that the L strain is more prevalent than the S strain and it is noted as being the more ‘aggressive’ strain which either transmitting more easily or replicating faster inside the body.
Coronaviruses are viruses that circulate among animals with some of them known to infect humans.
Bats are considered to be the natural hosts of these viruses but several other species of animals are also known to be a source.
The 2019 Coronavirus (COVID-19) has come from animals just like other coronaviruses.
 Where did Coronavirus (COVID-19) start?
Where did Coronavirus (COVID-19) start?The virus initially was first reported in Wuhan, Hubei Province, China in December 2019. However there are a couple of ‘theories’ of how the Coronavirus (COVID-19) exactly began.
Most of the initially infected many people were either those who frequently shopped or worked in the Huanan Seafood Wholesale market in the centre of Wuhan, China.
The Huanan Seafood Wholesale market also sells meat from other animals, including bats and snakes. The market was implicated in the COVID-19 spread in early January 2020.
The typical symptoms of coronavirus include fever and a cough that may progress to a severe pneumonia causing shortness of breath and breathing difficulties. However symptoms will vary from person to person.
Generally, coronavirus can cause more severe symptoms in people with weakened immune systems, older people, and those with long-term conditions like diabetes, cancer and chronic lung disease. See below for further information on at risk groups.
It has been stated that 81% of all Coronavirus COVID-19 illnesses were considered mild. (Li J et al. 2020)
According to the NHS as of 18 May 2020, the symptoms of coronavirus are:
Most people affected with coronavirus 2019 have at least one of the above symptoms. (NHS 111 Coronavirus COVID-19)
There are other symptoms such as
However please note that these symptoms don’t necessarily mean you have the Coronavirus (COVID-19). As you can see the symptoms are similar to other more common illnesses including a cold or the flu.
The WHO also state that other common symptoms of COVID-19 include
The WHO and the ECDC (European Centre for Disease Control) also state that some COVID-19 patients may also experience:
The symptoms will normally appear mild and begin gradually.
The American CDC also state that the symptoms may appear between 2-14 days after being exposed to the virus. However symptoms commonly appear around five (5) days. However these are only estimates and as more information and data that comes available, these estimates will be updated.
For those people who have the more serious case of COVID-19 they may develop severe pneumonia, sepsis, acute respiratory distress syndrome (ARDS) and septic shock which can lead in some cases to death. (ECDC Coronavirus 2020)
If you have a fever, cough or difficulty breathing you and all members of your household must self isolate for a minimum of 14 days (UK Government advice as of 16 March 2020). If your symptoms worsen please contact 111 or use the 111 coronavirus website.
For those of you in the U.K. if you think you have coronavirus COVID-19 and you are exhibiting symptoms, please use the online NHS 111 Coronavirus service. If you’re unsure whether you have coronavirus COVID-19 and you have symptoms please contact the NHS 111 to be safe.
The WHO have stated that some people can become infected with COVID-19 but then don’t go on to develop any symptoms nor do they feel unwell.
Your age is also no indication of how serious your symptoms would be if you were to develop Coronavirus COVID-19.
Unfortunately COVID-19 is a new illness and as of yet it is not known exactly how Coronavirus spreads between people. Coronavirus (COVID-19) is highly contagious and it is important to understand how it can spread.
What is known, is that other similar viruses are spread in cough droplets. The (American) Centre for Disease Control (CDC) say that COVID-19 is spread mainly from person to person. This is usually between people who are in close contact with each other and through respiratory droplets produced when an infected person coughs or sneezes or even talks.
These infected droplets can enter the body through the eyes, nose and mouth, either directly or after touching a contaminated object.
The CDC stated that it may be possible that someone can get COVID-19 by touching an object or a surface that has the virus on it, they then touch their own nose, mouth or their eyes.
However currently the scientists think that this is not the main way the virus spreads.
Overall, the COVID-19 virus appears to be spreading easily and ‘sustainably in the community’ otherwise known as “community spread” in some affected geographic areas. (Center for Disease Control and Prevention: Coronavirus questions and answers 2020)
According to the U.K. Government, as of 18 December 2020, “airborne transmission can occur in health and care settings in which procedures or support treatments that generate aerosols are performed. Airborne transmission may also occur in poorly ventilated indoor spaces, particularly if individuals are in the same room together for an extended period of time.”
In the U.K. if you are suspected to have coronavirus COVID-19 you are able to be tested for it via the NHS via swabs.
In the USA as of 5 March 2020 a specialised testing kit is now available to test for COVID-19 (Stanford News Centre 2020). The newly developed COVID-19 test kits will be used to test swab suspected Coronavirus COVID-19 patients. This new test kit is supposed to deliver the results within 12-24 hours.
If you are suspected to have coronavirus COVID-19, a health professional will take samples from your nose, throat and deeper respiratory tract and then send them for laboratory testing.
The samples are taken in the form of a swab which can be a combined viral nose and throat swab, or a viral nose swab and a viral throat swab, or they’ll take a a single swab used for throat then nose, or a nasopharyngeal aspirate.
As with all available tests it is not yet known how long a person has to be infected before the test comes back as positive.
According to the WHO, Public Health England (PHE) and the NHS anyone is at risk of getting coronavirus COVID-19.
The risk of how someone’s Coronavirus COVID-19 develops in them does depend on a number of factors including on your geographical location, your age, any underlying health conditions and can also depend on your occupation.
The WHO state that for most people the risk of someone developing coronavirus COVID-19 is low. However there are some groups of people who are at a higher risk of the virus becoming serious. For most people, if they do develop the disease the symptoms will usually be mild. (WHO, CDC, ECDC 2020)
The WHO stated in their report that most patients (77.8%) were aged 30 to 69 years (WHO Joint WHO-China Mission 2020).
However they did state that people of all ages can be infected by the coronavirus COVID-19, therefore there was no particular age group or bracket who is more susceptible than another.
Most people which is estimated to be around 80% of cases, recover from the disease without the need of special treatment.
For those people who are either living in or travelling to and from countries where the coronavirus COVID-19 has spread to, the risk of catching the disease is higher.
Approximately 1 (one) in 6 (six) cases of COVID-19 become seriously ill and go on to develop difficulty breathing.

There are certain groups of people who are at more risk of the Coronavirus COVID-19 developing into a serious illness. Those groups include the elderly, those with pre-existing long term conditions or those on immune suppresant medication.
Those in the at-risk group below are asked to stringently follow the social distancing guidance.
Please see below for further details on at risk groups and groups which we have received questions about. However please don’t panic or let your anxiety levels rise.
As of 30 March 2020, the U.K. Government announced that those in the at risk groups which include the elderly, those with serious health conditions and pregnant women are to strictly social distance (or ‘shield’). The full list of underlying health conditions is below.
Source: UK Government ‘Social Distancing to protect the elderly and those with vulnerable adults’ 16 March 2020
Source: UK Government ‘Guidance on social distancing for everyone in the U.K.’ Updated 30 March 2020
For those people over the age of 60 there is a high risk of developing a serious form of the disease. The risk factor does increase as the person’s age increases (World Health Organisation: Questions and Answers 2020).
For people with underlying long term medical problems such as (but not limited to) those listed below or those people who are on long term corticosteroids or other immune suppressing agents:
(Sources: WHO, CDC, HSE (Ireland))
Those people with pre-existing conditions such as those listed above have a much higher risk of COVID-19 developing into a serious illness.
In the first large study (Wei-jie Guan et al. 2020) of 1,590 patients from Wuhan found that those people who had one of the above underlying health conditions had a 79% greater chance of requiring intensive care or a respirator or both.
Newborn babies may become infected with the disease because of being in close proximity to an infected patient like most people. As of 12 March 2020 a newborn baby in the U.K. was the youngest person to be diagnosed with coronavirus COVID-19
Children can become infected with the virus and some can have a severe illness from it. According to the WHO they have said that children are not known to develop a severe form of the disease.
It has been found that children and young people can be affected by Coronavirus but they are considered as spreaders of the disease.
The WHO have reported that based on current research data available, there appears to be a relatively low incidence of coronavirus Covid-19 in those under 18 years of age. They made up only 2.4% of all reported cases (Begley, S. 2020)
At the moment only a small study has been done on pregnant woman transmitting the disease to their unborn child, however the study found that currently there is no evidence for intrauterine infection caused by vertical transmission in women who are infected with COVID-19 in late pregnancy (Huijun Chen, et al. 2020)
In the same study they also stated that “COVID-19 seems not to be especially severe in pregnant women, at least based on the small number in this study.”
UPDATE – However as of 30 March 2020 the U.K. Government have included pregnant women into the at-risk group and they have been asked to strictly follow social distancing guidance.
The U.K. Government have published guidance which has been updated on 11 January 2021 providing advice on shielding those people who are at extremely high risk of a severe illness from coronavirus COVID-19.
‘Shielding’ is a measure to protect people who are clinically extremely vulnerable by minimising all interaction between those who are extremely vulnerable and others. (Public Health England Advice)
Those people in this category are as follows:
Source: Public Health England ‘Guidance on shielding and protecting people defined on medical grounds as extremely vulnerable from COVID-19’
This advice regarding shielding is for your own personal protection, it is currently not enforced, meaning you don’t have to follow this guidance. However it is for your benefit and protection against the Coronavirus COVID-19. Therefore please strictly adhere to the social distancing rules.
The NHS will be in touch probably by letter with those people who are part of this group. However if you think you fall into one of the extremely vulnerable categories listed above please discuss your concerns with your GP or hospital clinician.
The current guidance as of 6 January 2021 is to stay at home at all times and only leave your home for any of the limited “reasonable reasons” listed. However this period of time could change, so please keep yourself updated with the latest guidance from the NHS and PHE.
Obviously those with CRPS will have serious concerns about the new coronavirus COVID-19, but it is important not to panic.
Unfortunately the coronavirus COVID-19 is still a new disease and experts are learning new information every day. However at the moment we do not know exactly how or if the COVID-19 will have a specific effect on someone who has Complex Regional Pain Syndrome (CRPS).
CRPS does affect the immune system as ‘high levels of cytokines (inflammatory chemicals) have been found in the tissues of people with complex regional pain syndrome. These cytokines do contribute to symptoms such as redness, swelling and warmth/heat that many CRPS patients experience’ (NINDS 2019).
There has been some research into finding out if CRPS is an autoimmune disorder and in a study (Dirckx, M. et al 2015) autoimmunity has been suggested as one of the pathophysiologic mechanisms that may underlie complex regional pain syndrome (CRPS).
In a recent study (Clark, JD. et al. Molecular Pain 2018) they conclude that “CRPS may involve both autoinflammatory and autoimmune components.”
Those people who have an autoimmune disorder or who have a poorly regulated immune system or who take immune suppressing medication do appear to have an increased risk of infections due to their greater immune dysregulation.
In some CRPS patients they find they have recurring infections suggesting they have a weakened immune system, meaning they have trouble fighting infections.
The health experts do emphasise that one of the main concerns for those who have an autoimmune disorder or those with a weakened immune system who contract COVID-19 is the secondary bacterial infection or the complications that may follow on from the original viral infection.
The British Pain Society have said in a message to the charity that some CRPS patients who are on long term corticosteroids or if you take other immune suppressing agents then you must be specially vigilant.
For those CRPS patients who have medication to help manage their pain and symptoms of complex regional pain syndrome, this may have an effect in different ways.
If you have opioid patches (transdermal opioids) to help manage your CRPS, there is a suggestion that if you were to develop COVID-19 and you have a fever or high temperature, it may increase the absorption from the patches leading to an increase of side-effects of them.
If you develop COVID-19 and you find your side effects from the patches are worsening, please speak to your treating doctor.
Generally opioids are often deemed to be immunosuppressant and cough-suppressants (they prevent cough) which may either delay or even mask the initial symptoms of COVID-19.
For those taking NSAIDs (Non-Steroidal Anti-inflammatories) it has been suggested in some research that there may be an increase in complications from simple respiratory infections or even a delayed recovery from the virus infection if you develop COVID-19.
According to the EFIC (European Pain Federation) and the WHO they have stated that they do not recommend against using ibuprofen. They are still in contact with medics regarding ibuprofen and at the moment they are not aware of any negative effects of ibuprofen on COVID-19 patients, other than the usual side effects. (EFIC 18 March 2020)
However the anti-inflammatory properties of Iburprofen may mask the signs and symptoms of COVID-19.
If you have confirmed COVID-19 or suspected of having it the British Pain Society recommend that you take paracetamol instead of ibuprofen. However if you take either NSAIDs or ibuprofen regularly as part of your medication regime you are advised to not stop taking them and speak to a medical professional if you are concerned.
According to the Expert Working Group on Coronavirus there is currently insufficient evidence to establish a link between use of ibuprofen, or other non-steroidal anti-inflammatory drugs (NSAIDs), and susceptibility to contracting COVID-19 or the worsening of its symptoms. (UK Government response to Ibuprofen 14 April 2020)
Unforunately the effect of corticosteroids on the immune system in people with COVID-19 is unknown, but possible concerns have been raised regarding reduced survival benefit and possible harms. (WHO March 2020)
If you develop COVID-19 you may experience a flare up of your condition and your symptoms. Please follow your pain management regime and also self management regime to help reduce your CRPS flare ups. Learn more about CRPS flare ups via our 5 Common Flare Up Myths and how to manage a flare up.
The current guidelines for the U.K. and most of the world is that you are to stay at home and only go out for food, health reasons, exercise or work (if you are unable to work from home)
There are a number of ways you can slow the spread of coronavirus COVID-19 and reduce the risk of developing the virus according to the NHS.
We understand that the virus enters your body through your mouth, nose and/or your eyes, therefore it is important to avoid touching your face with unwashed hands.
£8.50
The NHS and WHO guidance to reduce the risk of developing coronavirus COVID-19 is as follows:
If you are in the United Kingdom and you think you may be infected with Coronavirus COVID-19 it is important to self-isolate for 14 days and if your symptoms worsen you are advised to then seek medical help immediately by visiting the NHS 111 Coronavirus website to answer some questions online. If you don’t have access to the internet please call 111.
As of 16 March 2020 the U.K. government have said “anyone who shows certain symptoms to self-isolate for 14 days as well as all those in the same household, regardless of whether they have travelled to affected areas.”
The NHS 111 is for those living in England, Scotland, Wales and Northern Ireland. For those people in Scotland they are also advised to contact their GP surgery or NHS 111 if the GP surgery is closed.
For those of you in the UK you must use the NHS 111 service:
For those outside the U.K. it is important that you follow the instructions of the health professionals in your country.
As you can understand this is an ever changing situation and guidance is changing all the time around the world.
As of January 2021, the lockdown guidance has been changed to put the U.K. back in lockdown. That guidance is as follows:
You also need to
Social distancing is a set of steps you can take to reduce social interaction between people. This is to try to reduce the transmission of coronavirus COVID-19.
The new social distancing will also be called ‘Staying alert and staying safe.
‘Guidance on staying alert and stay safe (social distancing)’ PHE and UK Government 11 May 2020
When you go outside you should stay 2 metres (6 feet) away from other people.
When you return back home from going out for the above named reasons please wash your hands as soon as you get back home. Remember that you can spread the virus even if you don’t have symptoms.
For those being shielded, the ease of restrictions is being looked into at all times. However the current guidance updated 11 January 2021 for those being shielded is as follows:
Stay Home – Protect the NHS – Save Lives
If you know or think you have had coronavirus COVID-19 and you’re in the United Kingdom, you are asked to complete the NHS 111 coronavirus survey.
The purpose of completing the survey is to help the NHS learn more about this virus and where in the country people are developing it.
To complete the survey please click on the link below
NHS Coronavirus Status Checker
If you have symptoms of coronavirus COVID-19 and you have to stay at home, some employers are asking for a medical note. You can now get an ‘isolation note’ on the NHS 111 website.
The 111 website say that if you have to stay at home but feel well enough to work you can ask your employer if you are able to work from home. If you are able to work from home, you will not need an isolation note. If you’re unable to work from home then you are able to use the NHS 111 isolation note service.
NHS 111 Isolation Note
As of 11 May 2020, the UK Government in particular England have now advised to wear face masks or face coverings under the lockdown easement plans.
They state that people should “aim to wear a face-covering in enclosed spaces where social distancing is not always possible and they come into contact with others that they do not normally meet“. That would include, for example, on public transport and in some shops.
Scotland have advised the use of face coverings. However Wales and Northern Ireland also now recommend the use of wearing face masks.
The WHO still only recommend the use of surgical face masks for those either with coronavirus or for those working directly with coroanvirus infected patients.
If you are infected with the virus then wearing a surgical face mask may reduce the risk of you infecting others.
For face masks to be effective they need to be work correctly, frequently changed, removed properly and then disposed of safely.
The healthcare workers directly working with COVID-19 patients will use the most protective face masks which are FFP3 or N95.
It is difficult to know which masks offer what amount of protection. Many people are using homemade face masks they are obviously going to be unregulated and untested unlike those purchased from pharmacies and for healthcare. However there is plenty of advice on the internet on how to make these masks.
The European CDC have stated that reusable cloth masks are not recommended and may increase the chance of infection. (ECDC 26 March 2020 Cloth Face Masks)
However the US CDC states that cloth face coverings should:
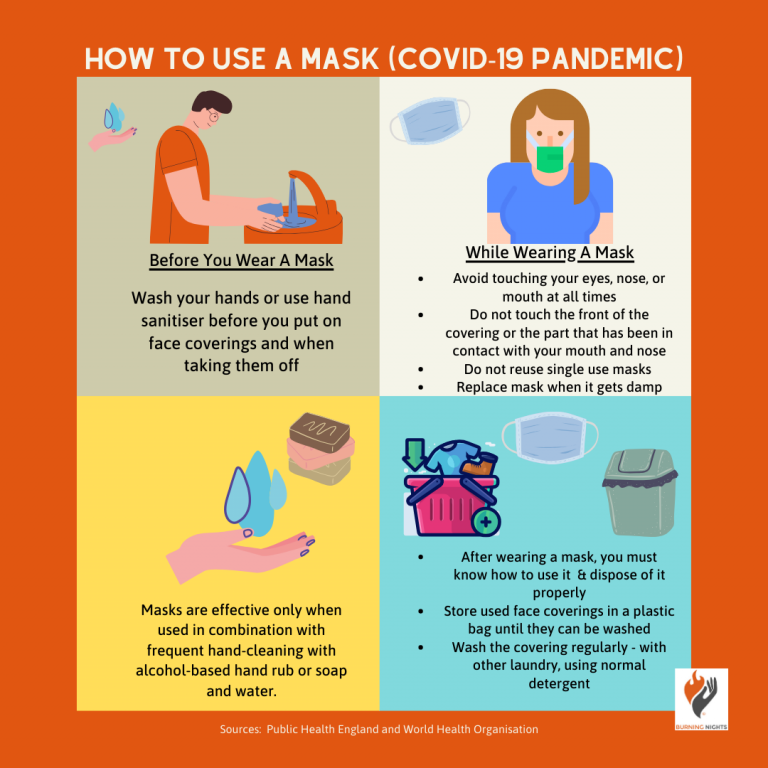 Since the U.K. Government advice change for people in England on face coverings, the PHE have said that people should wash their hands or use hand sanitiser before putting face coverings on and taking them off.
Since the U.K. Government advice change for people in England on face coverings, the PHE have said that people should wash their hands or use hand sanitiser before putting face coverings on and taking them off.
Additional advice includes:
The U.K. Foreign Office still currently advises against all but essential travel. If you do travel you must maintain the 2 metre (6 feet) distance where possible.
If you do travel you must consider wearing a face covering and gloves. Some airports have already made this compulsory. Please check with your airport if you are preparing to travel.
However from Monday 8 June, if you do travel, most travellers arriving in the UK including U.K. citizens by plane, train or ferry will be asked to provide a UK address where they must self isolate for 14 days. Surprise visits will be made to ensure you are self isolating.
If you don’t provide an address the government will arrange accommodation at the travellers expense. Passengers must use their own car to get to the destination rather than public transport.
As the coronavirus COVID-19 is a new disease there is no vaccine, no antiviral medication or specific treatment to cure it. Unfortunately vaccines can take many months or years to develop. Therefore at the moment the U.K. Government and WHO advice is to try and reduce the risk of the virus spreading and of you developing it by following their advice.
There are some possible drug treatments and vaccines under investigation and are being tested in clinical trials.
For those who are affected with the virus should receive appropriate care to relieve any symptoms they may be showing.
If you wish to track the cases of Coronavirus COVID-19 in the U.K. including the number of cases, where those cases are and the number of deaths in the U.K., you can track them via the Public Health England website.
If you have tested positive for COVID-19, the health authorities such as Public Health England (PHE) will then attempt to trace and contact everyone who you have been in contact with. This is called contact tracing.
If there is any chance you could have coronavirus whether you have travelled to an affected area or country, or you have been in close contact with an infected person, or if you have any of the symptoms you will be asked to self isolate. This means that you should stay away from other people and stay indoors. The U.K. have said you do not need to call NHS 111 to go into self-isolation.
As of 10 May 2020 the U.K. Government have stated that if you live with others, and you have a high temperature and/or a new continuous cough, you are asked to self isolate. If you live with other people, all members of your household are also asked to self isolate.
If you live alone you are to self isolate for 7 days after symptoms started. After 7 days, if you do not have a high temperature, you do not need to continue to self-isolate. If you still have a high temperature, keep self-isolating until your temperature returns to normal. You do not need to self-isolate if you just have a cough after 7 days, as a cough can last for several weeks after the infection has gone.
Please see the ‘Stay At Home: Guidance for households’ from the PHE for more information on the exact guidelines if you do develop coronavirus COVID-19.
To self isolate you should do the following things for up to 14 days to reduce the possible spread of the virus:
(Sources: PHE, NHS, ECDC, CDC)
You must follow the latest Government advice for self-isolation such as the U.K. Government PHE Home Isolation Guidance (Public Health England: Home Isolation 2020).
If you are in self isolation you must keep monitoring your symptoms.
For those of you who are in the U.K. the PHE advice if you are tested for coronavirus COVID-19 and you have a negative result and you have travelled to a specific country or area in Category 1, the latest PHE advice is to continue self isolation until you have been back in the UK for 14 days even if your symptoms have gone.
If you have just returned or travelled from a Category 2 country the latest U.K. Government advice is to carry on with self isolation until either your symptoms have gone or you have been back in the U.K. for 14 days, whichever is sooner (Public Health England: Home Isolation 2020).
Please do continue to update yourself as to the latest health authority (NHS 111) or Government advice as the coronavirus COVID-19 situation is constantly evolving.
We have produced a separate article on coronavirus (COVID-19) and your mental health with some tips and advice on how to cope and support your mental wellbeing when in self-isolation or when social distancing.
The coronavirus COVID-19 global health emergency can have an effect on your mental health. Increase in stress, anxiety or depression can all effect your Complex Regional Pain Syndrome (CRPS) and can cause your condition to flare up. Learn more about flare ups and how to reduce them via our 5 Common Myths of CRPS Flare Ups.
Try to look after yourself and give yourself some time for self care. It’s important to keep yourself calm and not to panic. Remember that this will end.
Although keeping informed as to the latest guidance is important, try not to overthink scenarios, or make assumptions or think of ‘will I get coronavirus’ type of questions. Speculation can only increase your levels of anxiety and stress.
It is a good idea to use various techniques to reduce your level of worry, stress and anxiety such as:
As you can see the global health emergency of the novel coronavirus – COVID-19 is constantly changing as is the advice from Government and health authorities.
Burning Nights CRPS Support has been in contact with the British Pain Society (BPS) to enquire if there is any specific information for those living with CRPS. Unfortunately there is no specific information other than the advice from the NHS and Public Health England (PHE). If this changes we will update this.
We have been told that if anyone is elderly, has a pre-existing long term condition, on long term corticosteroids or other immune suppressing agents, you must be especially vigilant.
It is important that you follow the hand hygiene by washing your hands in hot water and soap regularly for at least 20 seconds to remove any traces of the virus on your hands.
However as we’ve mentioned above, it is common for Complex Regional Pain Syndrome (CRPS) patients to have a weakened immune system and the condition has an autoimmune or autoinflammatory element to their condition.
According to the data and research available, patients with a weakened immune system may become seriously ill from the coronavirus COVID-19.
Therefore to reduce the risk of developing the COVID-19 virus you must follow the health advice from the NHS and PHE if you’re in the U.K. or your own country’s advice.
The information contained in this Coronavirus COVID-19 article is intended to be used as general guidance only on coronavirus infection in relation to complex regional pain syndrome (CRPS).
If you require advice or specific guidance please consult your GP or if it’s in relation to coronavirus COVID-19 please contact the NHS 111 service.
Burning Nights CRPS Support is a small UK charity trying to improve life for anyone affected by the debilitating chronic condition; Complex Regional Pain Syndrome (CRPS) and the devastating effects it can have on not only the life of a patient with the condition but also to those around them.
We offer a number of services which include an evidence based website, a support helpline, online community, email support and social media support, an annual national conference, CRPS awareness and support products, fundraising support and access to legal support via our legal panel.
Please show your support for the work that we do by making a small donation or by fundraising.
Donate to Burning Nights CRPS Support
Written: 10/03/2020
Last Updated: 10/06/2020